In today’s consult, I got to meet the oncologist herself, Dr. Chiorean. This was unusual, as these visits are typically with a PA. I thought I’d jot down a recap while that chat is still fresh in my mind.
First, she’s having my oxaliplatin dose reduced. Sounds like this is a fairly standard step taken in the final infusions. In her delightful Romanian accent, Dr C explained how the chemo side effects increase over time. She moved her hand in a flat line, describing the initial infusions, and then angled her hand sharply up, to demonstrate the cumulative impact in the final 2-3 infusions.
She made this call after she heard me describe my increase in side effects after the last infusion. Cold sensitivity certainly increased for me, significantly. Also, she was curious to hear about my struggles when I returned to work too soon after that infusion, and she helped me identify brain fog as the big issue there — not being able to think clearly was very stressful for me, on those workdays. She said that brain fog is one of the many side effects from Oxaliplatin. The main risk she is concerned about is that these side effects can persist for several months … or longer. Hence the reduction in oxaliplatin today.
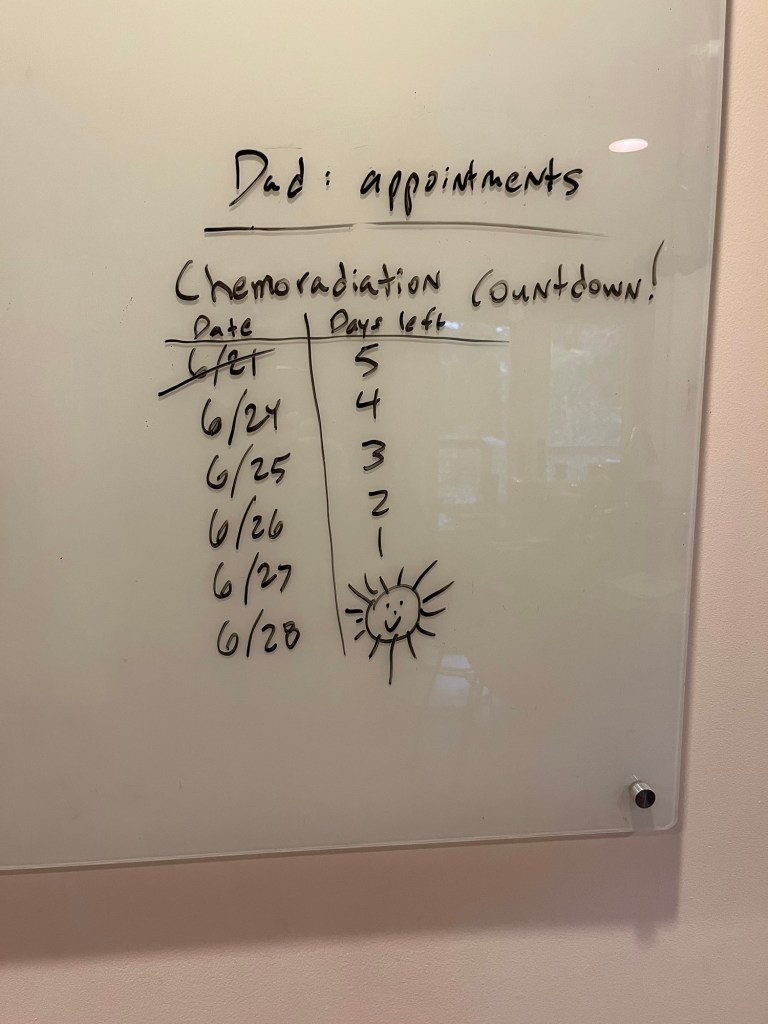
She also addressed my questions about scans. No; nothing was missed earlier in the year. She explained how the chemo and radiation phases really do work together; after the chemo is done, is when you assess the overall impact. She said the radiation is still doing its thing for six months after the radiation treatments stop, which I didn’t realize. Scans and sigmoidoscopy will occur at some point in December.
Regarding the surgery — there’s always the chance I won’t need it (we’ll see what the scans say). If it happens, she said it might not be until mid-January — but it’s not certain yet. She moved her hands out on each side: “plus or minus … many weeks.”
I did I get a call from the surgeon, Dr Atkinson, last week. She told me she’ll be going out on maternity leave in about three weeks, so it would not be her doing the surgery. She indicated more of a late December timeframe for the surgery. Dr C and Dr A need to meet and “align,” as everyone always says at my work.
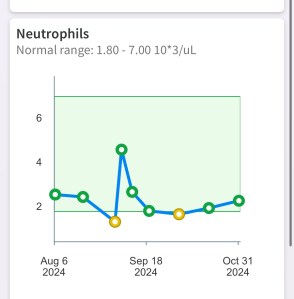
Fortunately, my neutrophils are increasing, which is what we want to see (if they get too low, as what happened before, the infusion gets delayed to a later date). So, it’s good to see that those accursed nivestym shots seem to be doing something.
I’ve been getting the oxaliplatin via IV over the past hour or so. I’m sleepy from the lorazepam, but have no fear: I won’t drink the chemo!