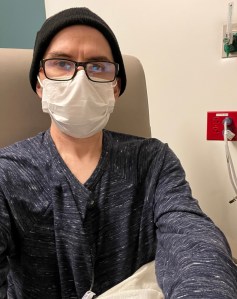
This round has hit me the hardest — particularly the last few days. Interestingly, the actual infusion day (last Thursday) was pretty uneventful. I felt surprisingly coherent as my friend Dorje gave me a ride home that afternoon. Pump disconnect day (Saturday) — which sometimes has been one of the more challenging days — also wasn’t too bad. The following Sunday and Monday, however — wow. Hard days, filled with periods of abject suffering: the typical mix of constantly-changing chemo effects (numbness, tingling, queasiness, sore throat) with some new elements: headaches, chest pain, and a weird extreme sore throat sensation that extended to my chest.
Cold sensitivity has increased, but that’s manageable and it’s the least of my worries. I have a system now where I always have a few glasses of water set out, so that they are at room temperature. Drinking water straight from the refrigerator is very unpleasant (feels like there are extremely cold shards of ice going down my throat). Also, I’m always wearing gloves when I head outside.
There’s a point where physical suffering is so extreme that you cannot distract yourself from it; it completely commands your attention and you’re just waiting for it to end. I was in that zone, over the last few days. Last night, I woke up at 1:30am and stayed awake through the remainder of the night. Lying down made things worse for me (I’ve had this before, a few times) — when I was lying down, the side effects were more extreme, especially with my throat (it felt like it was tightening). So, I couldn’t sleep until the side effects calmed down, which was 10 or 11am. It was a horrible night.
I know I have said this multiple times, but it strikes me how during these periods when I’m suffering through the effects of chemo, I do not feel like myself. My normal self is very planny, always striving, ticking through mental to-do lists. That self completely disappears, and is replaced with a zombie (as I often describe it) — prone to periods of staring, doing nothing. Also, certainly weirdly emotional. For example I read this article about Jenna Fischer and her experience with cancer, and that made me cry. I spend a lot of time just looking at art (in Facebook groups). I do not generally remember much of these days.
This afternoon, I believe I turned a corner for this cycle, and once again, started feeling like myself again. Still not 100%, but much better than the past few days. I am planning on returning to work tomorrow, unless I get hit with another sleepless night. My Mom recommended trying to sleep in a recliner (if I have more of the issues when I’m lying down); a good idea that I may try out tonight.
Only two more infusions to go! Next one is on Oct 31 … hmm, should I wear a costume?