I headed to Fred Hutch yesterday for chemo infusion #4, accompanied by my sister Katy. Lo and behold, after they drew my blood, they determined my white blood cell counts were too low for me to proceed with an infusion yesterday. They went ahead and rescheduled the infusion for next Wednesday, allowing time for my body to naturally build back up its white blood cells.
(By the way, check out Katy’s latest blog post about hiking, here!)
My care team is also going to have me increase the number of Nivestym shots that I self-administer, from 5 daily shots up to 7. While I don’t particularly enjoy sticking a needle into my belly (and the subsequent mild flu-like sensations, which last for 30-60 minutes), I understand the reason for doing this. I don’t want any future infusions to be canceled and rescheduled, if at all possible. This makes trying to maintain a work schedule incredibly difficult — not to mention the fact that Katy traveled up from Eugene, OR, for yesterday’s canceled appointment. Fortunately Katy was able to find a train south yesterday afternoon, but I still feel bad about the inconvenience of the cancellation.
So, yesterday was a day about learning to be flexible. To borrow a very over-used term in the world of corporate doublespeak, I had to quickly “pivot,” as did my sister, and change plans: travel schedule, work schedule, etc.
Also, in yesterday’s pre-infusion consultation, I ended up essentially in a negotiation about how things would proceed. I’m curious if this is common for other cancer patients, or not. I just felt I had to very actively advocate for myself, after the nasty mania experience of infusion #3. I presented a proposal:
- No more antihistamines; I seem to be unique in my strong negative reaction to these.
- Try the Oxaliplatin infusion back at the regular speed (the icing with mitts and gloves is pretty difficult to attempt for four hours).
- Keep the steroids at 50%.
- Let me take Ativan (lorazepam) as needed during the infusion process.
The nurse listened carefully and then went and discussed with the rest of the care team. When she returned, she explained they are hesitant to do everything I proposed, as they do want to mitigate the risks associated with Oxaliplatin. The fact is that I touched on their three primary levers for reducing these risks, namely: antihistamines, steroids, and reducing the speed of the infusion flow.
Their counter-proposal was to go ahead and cut the antihistamines, and keep the steroids at 50%, while keeping the Oxaliplatin at the reduced speed, like what they did last time. They explained they would like to see how I react to Oxaliplatin that way — using just one of the levers — before turning all three of them off. Also, they had no problem giving me Ativan up front, and indicated this is common for other patients. I found this to be reasonable and agreed to it.
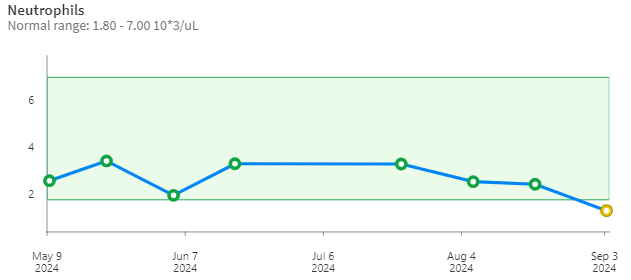
All of that discussion was before they determined my white blood cells (specifically neutrophils) weren’t high enough to proceed with a chemo infusion at all, yesterday. To get technical, my neutrophil count yesterday had dropped to 1.34 thousand neutrophils per microliter of blood, down from 2.46 a few weeks ago. While this was within acceptable range for Fred Hutch guidelines (they said their threshhold is 1), it was below the threshhold for the clinical trial I’m participating in, which I believe they said is 1.5.
So, I’ll be back at Fred Hutch next week, and need to update my work out-of-office requests, as all subsequent infusions will now shift to a different week. This does make me better understand why they don’t just schedule everything out in advance: chemotherapy treatment is not completely predictable, in terms of how individuals react over time.

Pingback: Infusion the Fourth | foiblish